Evaluating Telemedicine's Impact on Rural Healthcare Access

Telemedicine uses technology to deliver healthcare remotely, offering a lifeline to rural communities where access to care often falls short. You can see its impact in how it reduces travel burdens and connects patients to specialists without leaving their homes. During the Covid-19 pandemic, telehealth usage surged, and rural communities embraced it as a solution to healthcare access challenges. Today, 88% of rural respondents favor telehealth services, showing its potential to bridge the gap between urban and rural healthcare systems. With tools like Sobot’s Voice/Call Center, telehealth platforms can enhance remote healthcare delivery by improving response times and ensuring calls answered per hour (CAH) metrics remain efficient. Telemedicine transforms rural healthcare access, making healthcare more accessible and timely for underserved populations.
Challenges in Rural Healthcare Access
Geographic and Infrastructure Barriers
Long travel distances to healthcare facilities
Living in rural areas often means traveling long distances to access healthcare. Many rural residents face hours-long journeys to reach the nearest hospital or clinic. This creates significant challenges, especially during emergencies. For example, rural adults report higher transportation-related difficulties compared to urban residents, with 12% struggling to pay medical bills due to travel costs. These barriers widen the rural health disparity, leaving many without timely care.
Limited availability of specialized care
Specialized care remains scarce in rural regions. Patients requiring cardiology, oncology, or mental health services often need to travel to urban centers. This lack of access to care delays diagnoses and treatments, worsening health outcomes. According to recent data, 66.33% of Primary Care Health Professional Shortage Areas (HPSAs) exist in rural areas. This shortage highlights the urgent need for solutions like telemedicine to bridge the gap in rural healthcare.
Delayed Response Times
Impact on patient outcomes and emergency care
Delayed response times in rural healthcare settings can have life-threatening consequences. Rural hospital closures have led to an 8.7% increase in inpatient mortality rates. These delays affect emergency care, where every second counts. Telehealth usage has shown promise in reducing these delays by connecting patients to providers faster, improving outcomes in critical situations.
Addressing critical care delays in rural settings
Telehealth platforms play a vital role in addressing critical care delays. By enabling remote healthcare delivery, they reduce travel time and provide quicker access to healthcare professionals. This approach minimizes the rural health disparity and ensures patients receive timely care. Tools like Sobot’s Voice/Call Center enhance telehealth efficiency by streamlining communication and improving response times.
Resource Constraints
Shortage of healthcare professionals
Rural areas face a severe shortage of healthcare professionals. Over 66% of Primary Care HPSAs and 61.85% of Mental Health HPSAs are located in rural regions. This shortage limits access to healthcare and increases the workload for existing providers. Telemedicine helps alleviate this burden by allowing specialists to consult remotely, expanding access to healthcare for underserved populations.
Insufficient healthcare facilities and equipment
Many rural healthcare facilities lack the necessary equipment and infrastructure to provide comprehensive care. This limitation forces patients to seek treatment in urban areas, increasing costs and delays. Telehealth bridges this gap by offering remote healthcare delivery, reducing the need for physical infrastructure. Sobot’s Voice/Call Center supports this effort by ensuring seamless communication between patients and providers, even in resource-constrained settings.
Telemedicine's Role in Improving Access

Enhancing Response Times with Telemedicine
Real-time consultations and remote diagnostics
Telemedicine enables real-time consultations, allowing patients to connect with healthcare providers instantly. This feature proves especially valuable in emergencies, such as strokes or heart attacks, where every second matters. For example, a healthcare system in New York used telemedicine to manage minor emergency room visits, significantly improving response times. Remote diagnostics further enhance this process by enabling providers to assess symptoms and recommend treatments without requiring in-person visits. These advancements reduce delays and ensure patients receive timely care, even in rural healthcare settings.
Faster access to specialists through virtual platforms
Virtual platforms eliminate the need for patients to travel long distances to consult specialists. With telehealth, you can access cardiologists, oncologists, or mental health professionals from the comfort of your home. This approach not only saves time but also improves access to care for underserved populations. A recent survey revealed that 88% of rural respondents favor telehealth, highlighting its role in bridging the gap between urban and rural healthcare systems.
Expanding Access to Local Care
Bridging the gap for underserved populations
Telehealth bridges the gap for populations that struggle to access local care. Younger individuals and those in remote areas often face barriers to traditional healthcare. A survey of 200 rural residents showed strong interest in telehealth services, with many reporting positive experiences. This shift demonstrates how telemedicine can transform healthcare delivery, making it more inclusive and accessible.
Reducing the need for travel to urban centers
Telemedicine reduces the need for patients to travel to urban centers for specialized care. This change lowers travel expenses and minimizes the time spent away from work or family. For rural residents, this convenience translates into better health outcomes and fewer missed appointments. With telehealth usage increasing by 13% among rural populations, the benefits of remote healthcare delivery are becoming increasingly evident.
Integration with Customer Contact Solutions
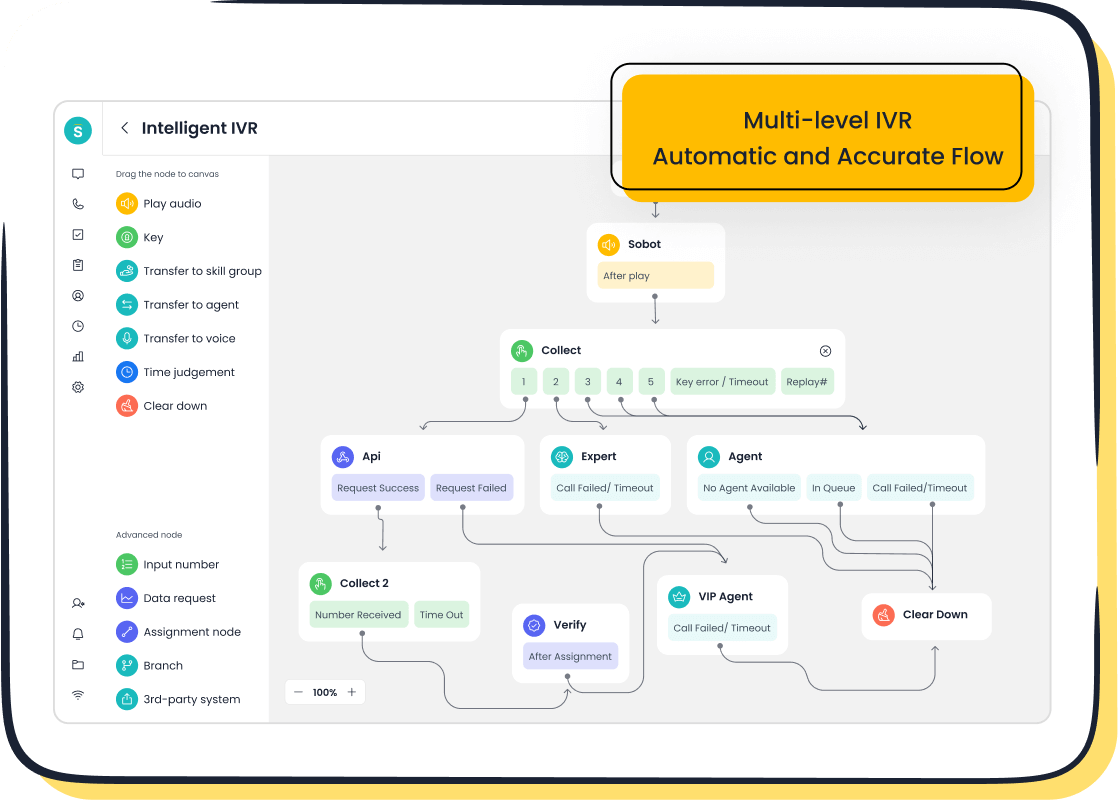
Role of Sobot's Voice/Call Center in telemedicine

Sobot's Voice/Call Center plays a crucial role in enhancing telemedicine systems. Its intelligent IVR and smart call routing ensure seamless communication between patients and providers. Features like real-time monitoring and AI-powered voicebots improve efficiency, making it easier to manage high call volumes. These tools support telehealth platforms by streamlining operations and ensuring patients receive timely assistance.
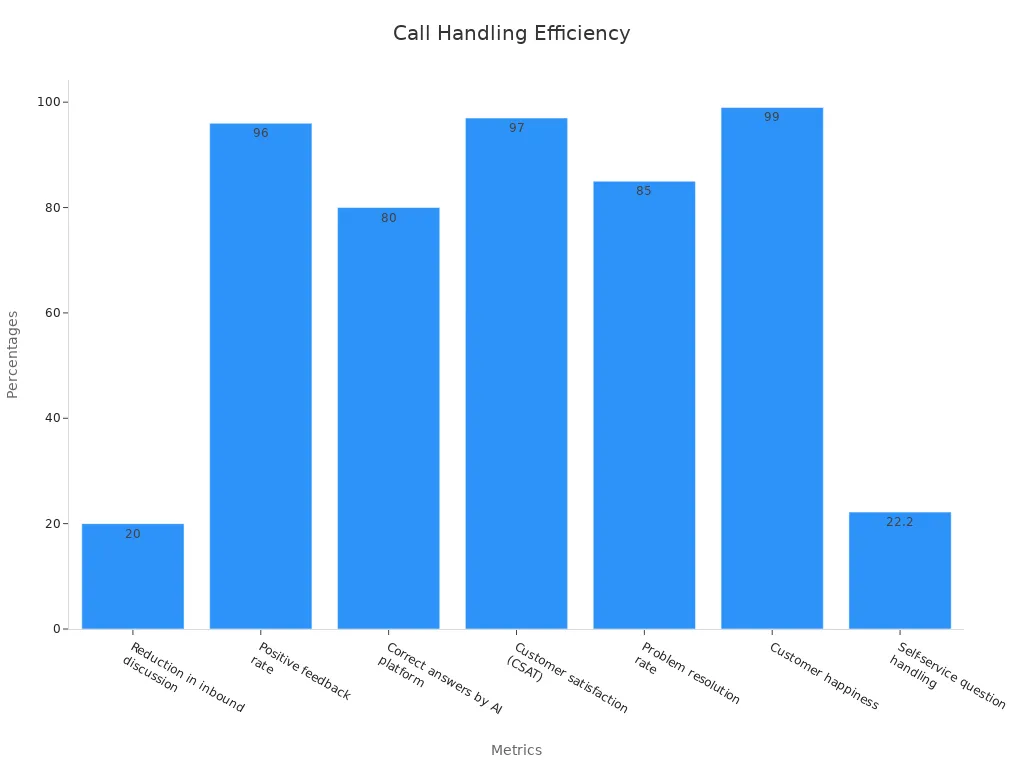
Calls answered per hour (cah) as a metric for efficiency
Calls answered per hour (cah) serves as a key metric for evaluating the efficiency of telemedicine systems. Sobot's Voice/Call Center excels in this area, with metrics like a 96% positive feedback rate and a 97% customer satisfaction score. These results highlight the platform's ability to handle calls effectively, ensuring patients receive the care they need without delays.
Patient and Provider Perspectives on Telemedicine

Patient Experiences
Convenience and reduced travel burden
Telemedicine has revolutionized healthcare for rural patients by eliminating the need for long-distance travel. You can now consult with specialists or primary care providers from the comfort of your home. This convenience reduces transportation costs and minimizes time away from work or family. A study revealed that telehealth usage significantly decreased patient transportation expenses and lost wages. Additionally, 88% of rural respondents expressed interest in telehealth, showcasing its growing acceptance. These benefits make telemedicine a game-changer for improving access to care in underserved areas.
Challenges with technology access and usability
Despite its advantages, telemedicine presents challenges for some patients. Limited internet access in rural areas and a lack of digital literacy can hinder its adoption. For example, older adults may struggle with navigating telehealth platforms, creating barriers to care. Addressing these issues requires investments in broadband infrastructure and user-friendly telehealth systems. Tools like Sobot’s Voice/Call Center simplify communication, ensuring patients can connect with providers seamlessly, even in areas with limited resources.
Provider Insights
Benefits for workload management and efficiency
Telemedicine has improved efficiency for healthcare providers. In Pennsylvania, providers reported reduced travel time to clinics, allowing them to see more patients. An EHR-based study in New York City found that over 600 providers experienced increased patient volumes after implementing telehealth. Metrics like clinician satisfaction and patient satisfaction highlight the effectiveness of telemedicine in streamlining operations. Sobot’s Voice/Call Center enhances this efficiency by offering features like smart call routing and real-time monitoring, enabling providers to manage workloads effectively.
Maintaining patient-provider relationships
Maintaining strong patient-provider relationships remains crucial in telemedicine. Virtual consultations allow providers to offer personalized care while reducing the physical distance between them and their patients. Many rural patients report feeling more comfortable discussing health concerns through telehealth platforms. This approach fosters trust and ensures continuity of care, even in remote settings.
Success Stories
Case studies from rural communities
In a rural Midwestern community, telemedicine initiatives have improved access to primary care. Patients reported increased comfort and a preference for telehealth over traditional visits. Government funding and programs like the interstate medical licensure compact have addressed barriers, making telemedicine more accessible. These efforts demonstrate how telehealth can transform rural healthcare systems.
Testimonials highlighting telemedicine's impact
Rural obstetric service providers have shared success stories about telemedicine’s role in maintaining maternity care. A 2020 case study emphasized the importance of community support and partnerships in overcoming challenges. Patients frequently highlight the convenience and improved access to care telemedicine provides, reinforcing its value in rural healthcare.
Financial and Operational Impacts of Telemedicine
Cost Savings for Patients and Providers
Reduced travel expenses for rural patients
Telemedicine significantly reduces the financial burden of travel for rural patients. Many individuals in remote areas face high transportation costs when seeking care in urban centers. By enabling virtual consultations, telehealth eliminates the need for these trips. A study revealed that rural patients saved on transportation expenses and avoided lost wages by accessing care locally. This shift not only improves affordability but also encourages patients to seek timely medical attention, addressing the rural health disparity.
Lower operational costs for healthcare facilities
Healthcare facilities in rural areas benefit from reduced operational costs through telemedicine. Traditional in-person care often requires extensive infrastructure and staffing. Telehealth platforms streamline operations by minimizing the need for physical resources. For example, rural hospitals can allocate funds more efficiently by leveraging virtual consultations and remote diagnostics. This approach helps sustain facilities that might otherwise face financial strain, ensuring continued access to care for underserved populations.
Economic Benefits for Rural Healthcare Systems
Increased patient retention in local systems
Telemedicine fosters patient retention within rural healthcare systems. Patients no longer need to travel to urban hospitals for specialized care, allowing local facilities to retain revenue. This retention strengthens rural health systems and reduces the financial losses caused by patient migration. Additionally, telehealth usage creates a professional network for providers, improving collaboration and treatment outcomes. Testimonials from rural providers highlight how telemedicine enhances trust and reassurance in care delivery.
Revenue growth through expanded telemedicine services
Expanding telemedicine services generates new revenue streams for rural healthcare systems. Local facilities benefit from increased patient visits, lab tests, and pharmacy services. The table below outlines the economic advantages of telehealth:
| Benefit Type | Description |
|---|---|
| Decreased patient transportation costs | Reduces the financial burden on patients, encouraging them to seek care locally. |
| Minimizing patient lost wages | Patients can maintain their income by avoiding time off work for travel to distant facilities. |
| Reduced hospital staffing costs | Telehealth can lower operational costs, allowing hospitals to allocate resources more efficiently. |
| Increased local lab and pharmacy revenues | Local healthcare facilities benefit financially from increased patient visits and services. |
Role of Technology in Cost Efficiency
Sobot's Voice/Call Center for operational optimization

Sobot's Voice/Call Center enhances telemedicine efficiency by optimizing communication workflows. Its intelligent IVR and smart call routing ensure patients connect with the right providers quickly. Features like real-time monitoring and AI-powered voicebots reduce inbound discussion time by 20%, improving overall productivity. These tools help healthcare facilities manage high call volumes while maintaining a 95% customer satisfaction rate.
Data analytics to improve healthcare delivery
Modern data analytics play a crucial role in improving healthcare delivery. Sobot's Voice/Call Center leverages analytics to track performance metrics such as call resolution rates and patient feedback. The chart below illustrates the platform's impact on cost efficiency:
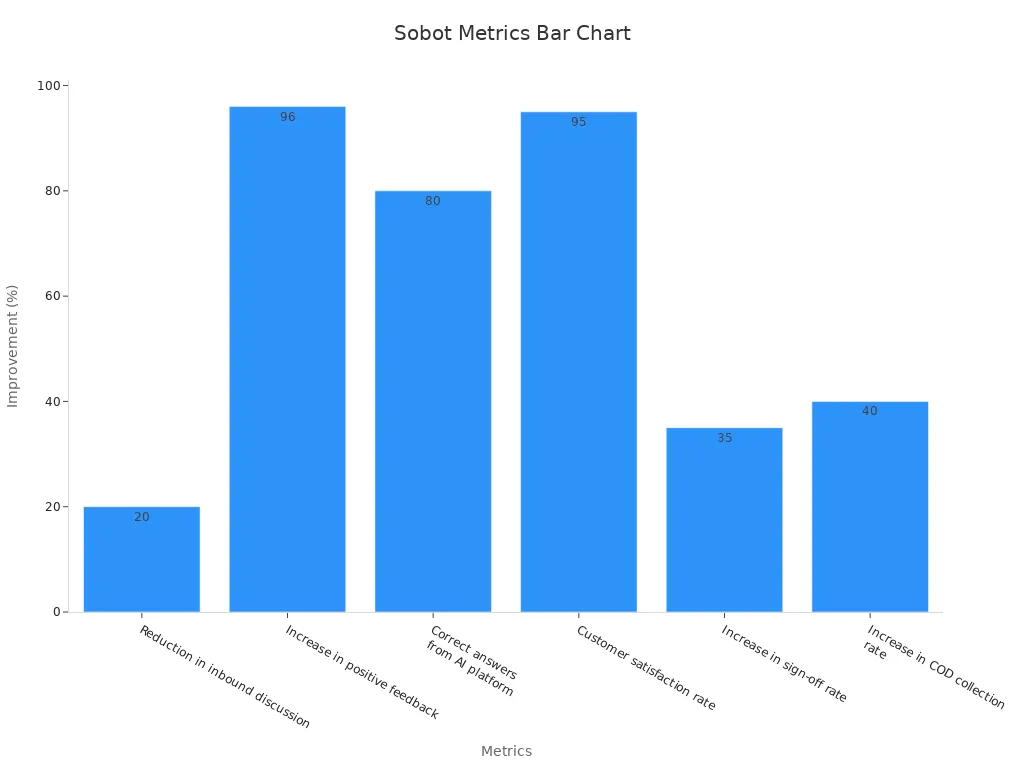
By analyzing this data, healthcare providers can identify areas for improvement and optimize resource allocation. This approach ensures better outcomes for patients while reducing operational costs, addressing the rural health disparity effectively.
Limitations and Challenges of Telemedicine
Technology and Connectivity Issues
Limited internet access in rural areas
Nearly 20% of the U.S. population lives in rural areas, where reliable internet access remains a significant challenge. Without stable connectivity, telehealth implementation becomes difficult, leaving many patients unable to access virtual care. This gap in infrastructure limits telehealth usage and creates disparities in healthcare delivery. Expanding broadband access in these regions is essential to ensure telemedicine reaches underserved populations.
High costs of telemedicine infrastructure
Building and maintaining telehealth systems require substantial investment. Rural healthcare facilities often struggle to afford the necessary technology, such as video conferencing tools and diagnostic equipment. These costs hinder telehealth implementation, especially in resource-constrained settings. Solutions like Sobot’s Voice/Call Center can help optimize communication workflows, reducing operational expenses and making telehealth more accessible.
Regulatory and Policy Barriers
Licensing and cross-state practice restrictions
The end of the COVID-19 Public Health Emergency reinstated stricter licensing requirements, complicating cross-state telehealth implementation. During the emergency, providers could practice nationwide without state-specific licenses. This flexibility ended, creating barriers for patients needing care from out-of-state specialists. Known as the "telemedicine parking lot phenomenon," patients now travel across state lines to access virtual care. Addressing these licensing challenges is crucial for expanding telehealth usage.
Privacy and security concerns with telehealth platforms
Privacy concerns also pose challenges for telehealth implementation. During the pandemic, relaxed HIPAA compliance allowed platforms to operate without meeting strict privacy standards. While this enabled rapid telehealth adoption, it raised concerns about patient data security. Ensuring telehealth platforms comply with privacy regulations is vital to maintaining trust and protecting sensitive information.
Adoption Challenges
Resistance to change and lack of digital literacy
Adopting telehealth faces resistance from both patients and providers. A study revealed that 46% of patients felt telehealth lacked personal contact, while 12.6% experienced technology-related issues. Additionally, 91.3% of providers reported technology challenges faced by patients, and 45.1% encountered difficulties themselves. These barriers highlight the need for user-friendly platforms and better education on telehealth usage.
Training and support needs for healthcare providers
Many rural providers lack the training needed for telehealth implementation. For example, 58% of mental health professionals in rural areas reported insufficient training to use telehealth effectively. This gap stems from the rapid adoption of telehealth during the pandemic. Offering comprehensive training programs and support systems can empower providers to deliver quality care through telemedicine.
Telemedicine has revolutionized rural healthcare by improving access and response times. You can now connect with specialists faster, reducing delays that often worsen health outcomes. Telehealth platforms, supported by tools like Sobot's Voice/Call Center, ensure seamless communication and efficient care delivery. For example, real-time call routing and monitoring enhance telehealth usage, enabling providers to manage high patient volumes effectively. However, addressing challenges like limited internet access and digital literacy remains essential. Tailored strategies, such as expanding broadband and offering user-friendly systems, can maximize telehealth's potential in underserved areas.
FAQ
What is telemedicine, and how does it help rural communities?
Telemedicine uses technology to deliver healthcare remotely. It helps rural communities by reducing travel time, improving access to specialists, and addressing healthcare shortages. For example, telehealth platforms enable real-time consultations, ensuring patients in remote areas receive timely care without leaving their homes.
How does Sobot's Voice/Call Center enhance telemedicine?
Sobot's Voice/Call Center optimizes telemedicine by streamlining communication. Its intelligent IVR and smart call routing connect patients to providers quickly. Features like real-time monitoring and AI-powered voicebots improve efficiency, ensuring seamless healthcare delivery even in resource-limited rural settings.
What are the main challenges of telemedicine in rural areas?
Limited internet access, high infrastructure costs, and digital literacy gaps are key challenges. For example, 20% of rural U.S. residents lack reliable internet, making virtual consultations difficult. Addressing these issues requires investments in broadband and user-friendly telehealth systems.
How does telemedicine reduce healthcare costs for rural patients?
Telemedicine eliminates the need for travel to urban centers, saving on transportation expenses and lost wages. A study showed rural patients saved significantly by accessing care locally. This affordability encourages timely medical attention, improving health outcomes.
Why is telemedicine important for rural healthcare systems?
Telemedicine bridges the gap in rural healthcare by addressing provider shortages and infrastructure limitations. It ensures timely care, reduces health disparities, and strengthens local healthcare systems. Tools like Sobot's Voice/Call Center further enhance its efficiency, making it a vital solution for underserved populations.
See Also
Understanding Medical Call Center Services And Their Advantages
Advantages And Disadvantages Of Working Remotely In Call Centers
Enhancing Call Center Efficiency Through Effective Monitoring Techniques